Neuroscientist Michael Cole Uses Machine Learning and Predictive Modeling to Help Patients With Cognitive Deficits
As a middle-schooler growing up in Napa, California, in the Bay Area, Associate Professor Michael W. Cole learned how to program his parents’ computer and went to tech expos with his father. As an undergraduate at University of California at Berkeley, he took computer science courses while working a side job at Apple Computer, figuring he’d become a software engineer.
Along with computers, though, Cole had always been interested in big-picture questions related to our existence, and at Berkeley he took courses in psychology, linguistics and philosophy as well, along with volunteering in a cognitive neuroscience research lab that changed his academic direction.
Then his father had a stroke just before Cole was due to graduate.
"I just kept thinking how foundational the human brain is to our existence and, from a philosophical angle, how this chunk of meat in our heads determines who we are and our entire experience,” said Cole. “My dad’s stroke got me thinking about the brain’s practical aspects, and I became interested in solving its mysteries.”
Cole went on to obtain his PhD in neuroscience at the University of Pittsburgh and Carnegie Mellon, and arrived at Rutgers University–Newark in 2014 as part of the Center for Molecular and Behavioral Neuroscience (CMBN) after completing a postdoctoral fellowship at Washington University in St. Louis.
Since then, Cole has established himself as a formidable researcher uncovering how the brain works and the behavioral implications of various brain functions. He’s especially interested in the network connectivity of various regions of the brain, and the cognitive and neural mechanisms that make human behavior flexible and goal-directed.
Cole and his team of researchers at the Cole Neurocognition Lab do this using a variety of techniques, applying network science, computational modeling, and machine learning approaches to data collected from the human brain (with fMRI and other imaging techniques) and conducting neural network simulations. By focusing on cognitive control and the dynamics that play out among regions of the brain, they can examine network disruptions underlying various brain and mental disorders like schizophrenia, OCD and bipolar disorder, laying the foundation for new approaches to treating these illnesses.
“I don't have a clinical degree. I do fundamental research, looking at how things work, but it’s important that we keep a pathway open into clinical and applied research,” said Cole. “How the brain works and the clinical implications are both interesting and important."
Cole’s team recently helped with a study looking at a pressing mental health issue that’s been making news: opioid addiction.
Using machine-learning techniques, they performed analysis on data collected by Rutgers Biomedical and Health Sciences (RBHS) researchers. That study used a new and improved diagnostic method to identify and distinguish between brain structure and functional connectivity in opioid-addicted patients and healthy, non-addicted subjects. The improved diagnostics could lead to better treatment and outcomes for those with opioid addiction.
But it’s his lab’s research related to schizophrenia that Cole believes is some of its most important, given how the cognitive and behavioral deficits—auditory hallucinations, language problems and disordered thinking—impact patients’ ability to perform everyday tasks and follow instructions to accomplish new tasks.
“Schizophrenia takes a much bigger toll than most people realize,” said Cole. “Only 1 percent of all humans have it, and that doesn’t seem like a lot, but it is if you think about how that translates to, say, COVID. A low mortality rate still means an awful lot of people when you apply it to all 7.9 billion humans.”
There’s also a huge connection between schizophrenia and homelessness and unemployment, according to Cole. And the age of onset is usually the early 20s, affecting affects patients much longer than conditions like Alzheimer’s, which translates into a huge impact on families, the economy and our healthcare system.
To that end, Cole’s team has been breaking ground with a unique approach to studying brain network connectivity and functioning as it applies to schizophrenia: a technique called “activity flow mapping,” which examines how activity moves in the brain, and the type of brain-region connectivity patterns that occur, when the brain is both at rest and doing tasks.
Schizophrenia patients typically suffer from connectivity dysfunctions. Cole’s idea, which he’s been working on since 2014, is to create models from these brain-connectivity patterns between regions of the brain—models that can actually predict activity flow downstream—and then intervene to alleviate connectivity dysfunction in these patients.
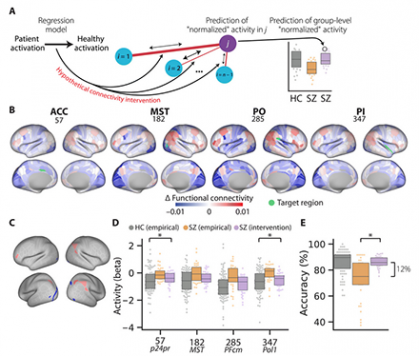
In a paper published this summer in the journal Science Advances, he and his team reached something of a milestone: They not only reiterated how activity-flow models can accurately predict task-related brain activations in both simulated and empirical data from healthy young adults, but they showed how those same models can accurately predict aberrant cognitive activations across multiple brain networks. The team then simulated a connectivity-based clinical intervention, predicting specific treatments that actually normalized brain activations and behavior in schizophrenia patients.
“The activity-flow methodology is predictive but also generative: You take someone’s brain connectivity and produce an artificial network model to see how it will generate activity in brain regions, the idea being that we can change connections in the model and see what would likely happen if we changed those connections in a real human brain,” said Cole. “This is the first time we’ve actually made a hypothetical treatment, simulated an intervention in a model that made predictions from each subject's brain data," said Cole. “The treatment may actually work as-is, though no model is perfect and needs to be tested.”
Cole says that his next step would be to test his hypothetical treatment in actual patients but that it’s hard to change brain connectivity systematically, so more work needs to be done, especially to do it reliably. At the same time, he acknowledges that seven years in, he and his team have come a long way with their research, and he’s excited about the challenges that lie ahead.
“We’re making progress in understanding how the brain works and what goes wrong in patients with schizophrenia and other conditions, and we’re hopeful we'll see some of the practical benefits of this research in the not-too-distant future,” said Cole. “Like most fundamental research, it's more about understanding so foundational that it'll have many unforeseeable benefits, with a lot of those benefits felt far down the road.”



